Mouth ulcers, also known as oral ulcers or canker sores, are a common yet uncomfortable ailment. These painful mouth sores make eating, drinking, and speaking difficult. Whether you’ve had ulcers once or often, recognizing their origins, symptoms, and treatments is essential for comfort and dental health. This talk will cover mouth ulcer kinds, causes, symptoms, and treatment options. In this article, we will discuss the causes of canker sores and the steps you can take to treat them for a more pleasant mouth.
Mouth Ulcers – What Is It?

According to the National Health Service (NHS), mouth ulcers are small, painful sores that form on the mucous membranes inside the mouth. Also, mouth sores, which are called mouth ulcers or stomatitis, can look different based on what caused them. They are round or oval and have a white or yellowish middle with a red rim. These ulcers can happen alone or in groups, and they usually last between 1-2 weeks before they heal on their own.
Causes of Mouth Ulcers
Mouth ulcers, which are also called mouth ulcers or canker sores, can be caused by many different things. Even though it’s not always clear what causes mouth sores, they are often linked to:
- Minor Injuries: Traumatic ulcers may result from toothbrush abrasions, accidental bites, or dental appliance damage.
- Immune System Dysfunction: The immune system erroneously assaults healthy mouth cells, causing minor and large aphthous ulcers.
- Viral Infections: Mouth sores can be caused by some viruses, like the herpes simplex virus (HSV). Most of the time, these sores hurt and come back.
- Nutritional Deficiencies: Lack of important nutrients like vitamin B12, iron, or folic acid can cause mouth sores.
- Hormonal Changes: Some people get mouth sores when their hormones change, like when they have their period or are pregnant.
- Stress and Emotional Factors: Anxiety or emotional stress can weaken the immune system and make people more likely to get mouth sores.
- Food Sensitivities: Some foods, like hot or acidic foods, citrus fruits, or chocolate, can cause mouth sores or make them worse in some people.
- Certain Medications: Antibiotics, immunosuppressants, and nonsteroidal anti-inflammatory medicines (NSAIDs) may cause mouth ulcers.
- Systemic Diseases: Mouth ulcers may result from systemic diseases including IBD, Behçet’s illness, or HIV/AIDS.
Diagnosis of Mouth Ulcers
Healthcare experts can do the following to identify mouth sores and find out what’s causing them:
- Physical Examination: To determine ulcer size, location, and appearance, a dentist will examine the mouth and oral tissues.
- Medical History: Your medical history, including underlying diseases, medications, and nutrition, might assist uncover ulcer causes.
- Biopsy: If the ulcers are chronic, big, or suspicious, a biopsy may be conducted to rule out more severe disorders.
- Blood Tests: These can be done to check for food deficits or to see if mouth sores are caused by illnesses that affect the whole body.
- Allergy Testing: It may identify probable allergens if mouth ulcers are caused by an allergic response.
So, if mouth ulcers last more than 2 weeks are abnormally big, cause significant pain or other symptoms, or interfere with eating or drinking, visit a doctor. Based on the mouth ulcers’ symptoms and etiology, a doctor can diagnose and treat them.
Types of Mouth Ulcers
Mouth ulcers, also known as oral ulcers or canker sores, can cause pain and irritation. Based on their causes and features, they are divided into several categories. Knowing the forms of mouth ulcers helps identify symptoms, find treatment, and prevent recurrence. Now, we’ll discuss mild and large aphthous ulcers, herpetiform ulcers, traumatic ulcers, drug-induced ulcers, and systemic disease-associated ulcers in this article. These kinds may help you understand mouth ulcers and how to treat them:
Canker Sores
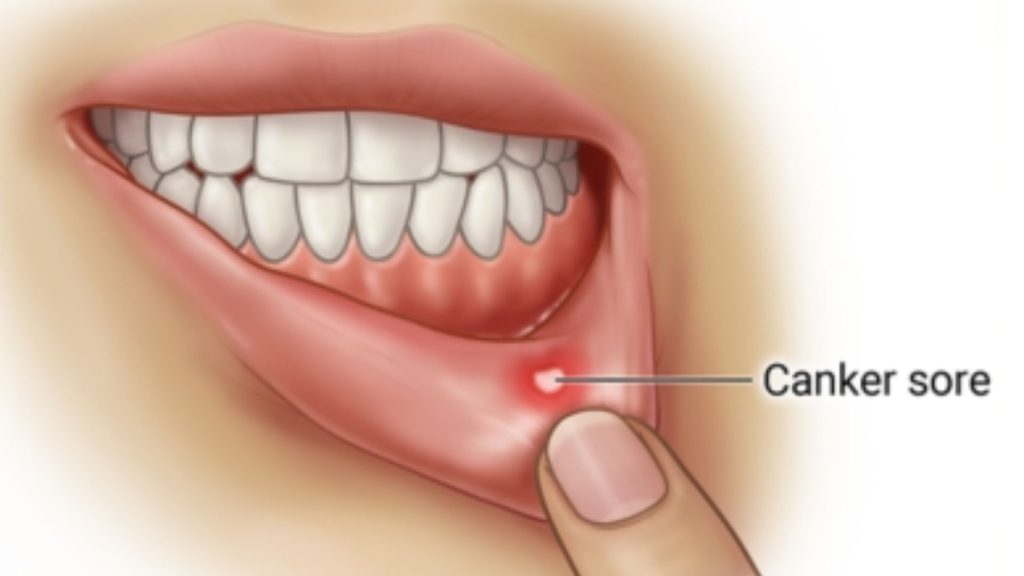
Common mouth sores include canker sores, commonly known as aphthous ulcers. They usually look like small sores that are round or oval and have a white or yellowish middle and a red edge. Canker sores may range from a few millimeters to 1 centimeter. Canker sores are usually small and appear on the inside of the lips, cheeks, or under the tongue. They may hurt while eating, drinking, or cleaning teeth. Sometimes clusters of canker sores emerge. Several causes may induce canker sores, including:
- Accidental biting or dental appliance irritation.
- Hormonal or emotional stress.
- Deficiencies or foods.
- Weakened immunity.
- Genetic tendency.
Overall, canker sores heal without scarring in 1–2 weeks. Oral creams or mouthwashes that you can buy over the counter and that contain calming agents or protective ingredients can help relieve pain and speed healing. Consult a doctor if you have big, chronic, or recurrent canker sores.
Cold Sores

Cold sores are caused by the herpes simplex virus (HSV), primarily HSV-1. They’re a frequent viral illness that affects the lips, nose, chin, and cheeks. Information on cold sores:
- Appearance: A tingling or burning feeling precedes the production of tiny, fluid-filled blisters. These blisters may be red or large and clustered. Blisters may rupture, exude clear fluid, then crust over after a few days. Crusts recover after 7–10 days.
- Contagiousness: Cold sores spread easily. The blister fluid or contaminated region might propagate the infection. To prevent the transmission of the virus, avoid kissing, sharing utensils, and oral activities.
- Triggers: Herpes simplex virus carriers may have cold sores from certain conditions. These triggers may include stress, disease, a compromised immune system, hormonal changes, exposure to sunshine or cold temperatures, or physical damage to the afflicted region.
- Treatment: The herpes simplex virus cannot be cured, although several therapies may control cold sore outbreaks. Antiviral lotions like docosanol or acyclovir may lessen symptoms and speed up recovery. For severe or regular outbreaks, doctors may give pill-form antivirals.
So, if you have cold sores, see a doctor for a proper diagnosis and treatment. They can help manage epidemics and limit transmission.
Herpetic Gingivostomatitis
Herpetic gingivostomatitis is a viral illness that mostly affects the mouth and gums. HSV, usually HSV-1, causes it. Here’s information about herpetic gingivostomatitis symptoms: Painful, tiny, fluid-filled mouth and gum blisters or ulcers.
- Gum inflammation (gingivitis).
- Sore throat, trouble swallowing.
- Fever, malaise.
- Neck lymph nodes that swell.
Since herpetic gingivostomatitis is very infectious, thus it’s crucial to avoid its spread. This involves regular handwashing, avoiding close contact with people with current outbreaks, and not sharing toothbrushes or utensils.
Oral Thrush

Oral candidiasis, or oral thrush, is caused by Candida yeast overgrowth in the mouth. Candida is a natural mouth resident, However, some conditions might cause an imbalance and oral thrush. Here are oral thrush symptoms.
- Plaques or creamy white areas on the tongue, inside cheeks, roof of the mouth, gums, or tonsils.
- Localized pain.
- Taste impairment.
- When scraped or rubbed, patches may bleed.
If you think you have oral thrush, see a doctor or dentist so you can be properly diagnosed and given the best course of therapy. They can advise on infection management and identify causes.
Hand, Foot, And Mouth Disease

Hand, foot, and mouth disease (HFMD) is a viral illness that mostly affects newborns and children but may also impact adults. It is caused by various viruses, most notably coxsackievirus A16 and enterovirus 71. Here are some symptoms of hand, foot, and mouth illness:
- Fever, generally mild to severe.
- Sore throat and difficulty swallowing.
- Painful mouth, tongue, gum, and throat blisters.
- Rash on the palms, soles, and sometimes the buttocks.
Hand, foot, and mouth disease is a viral illness that normally goes away without therapy. However, symptom relief is possible:
- Hydrating to avoid dehydration.
- Reducing heat and discomfort using OTC painkillers.
- Soft meals and avoiding spicy or acidic foods that might cause mouth sores.
If Oral Ulcers Aren’t Treated, What Happens?
Mouth sores are a pretty normal and everyday problem. It’s crucial not to disregard mouth ulcer therapy since it may cure on its own in a few weeks. Because untreated mouth ulcers may cause serious health issues and lower quality of life. So, what happens if oral ulcers aren’t treated?
- Pain and discomfort: If you don’t treat the condition, it may keep coming back and the pain may get worse and worse.
- Infection: Mouth sores invite germs and viruses, producing infections. Untreated, it may cause ulcer inflammation, swelling, and pus, increasing the risk of infection spreading.
- Nutritional imbalances: Pain and discomfort may make eating and swallowing difficult. If you don’t treat oral ulcers, you may not acquire enough nutrients and become malnourished.
- Speech and communication disorders: Mouth ulcers may make talking painful. Untreated, you may have trouble communicating, affecting your social life.
- Impact on quality of life: Eating, talking, and sleeping pain may disrupt everyday life, work, and social relationships.
So, it is important to treat mouth sores as soon as they show. If you have signs of mouth sores, see your doctor or dentist for help and treatment.
Healing From Mouth Sores: Possible Therapies
Mouth ulcer treatment depends on kind, severity, and etiology. Most mouth ulcers heal on their own in 1-2 weeks, but some treatments may relieve symptoms, speed healing, and prevent recurrence. Common treatments:
- Topical Medications: Topical pain relievers and mending aids, like mouth rinses, creams, and ointments, can be bought without a prescription or over-the-counter. Some of the ingredients in these items could be benzocaine, lidocaine, or hydrocortisone. They can be put on the sores directly several times a day or as told by a doctor or nurse.
- Oral Analgesics: Pain medicines you can buy over-the-counter, like aspirin or ibuprofen, can help with mouth sore pain and inflammation. Follow the dosage instructions and talk to a doctor or nurse if you have any other health problems or are taking other medicines.
- Steroid Therapy: Healthcare practitioners may administer corticosteroids as topical or oral treatments for severe mouth ulcers. These may decrease inflammation, relieve symptoms, and speed up recovery. Systemic corticosteroids’ adverse effects need close monitoring.
- Management of Underlying Conditions: If mouth sores are caused by an underlying systemic condition, it’s important to control and treat that condition properly. To create a complete treatment plan, rheumatologists, gastroenterologists, and immunologists may collaborate.
So, for mouth ulcer diagnosis and treatment, see a dentist. They may assess your condition, prescribe therapies depending on ulcer type and severity, and advise on controlling symptoms and avoiding recurrence.
Conclusion

In short, we’ve learned about the different kinds of mouth ulcers, what causes them, how to spot the signs and how to effectively identify and treat them. Knowing about mouth sores makes us understand how important it is to take care of our teeth. However, expert dental assistance is necessary for correct diagnosis and treatment. The high-quality competence at Spring Orchid Dental is one of the main advantages of frequent dental checkups. Experienced dentists work here. They use cutting-edge techniques and have considerable dental expertise to assure your safety and efficacy.
Additionally, Spring Orchid Dentistry Clinic prioritizes patient comfort and safety. When you go to the clinic, you will feel safe and sure because it is clean and has modern equipment.
FAQs
Can Too Much Vitamin C Cause Mouth Ulcers?
No, too much vitamin C does not cause mouth ulcers, but a vitamin C shortage does. Vitamin C boosts the immune system and heals wounds, which may help prevent mouth sores and speed up their recovery. But, too much vitamin C or a high dose can cause gut pain, diarrhea, or both. These signs could make the stomach upset and lead to mouth ulcers.
Do Mouth Ulcers Turn White When Healing?
Yes, mouth ulcers usually become white while healing. A fibrin clot—a white or yellowish-gray film—may grow over the ulcer as it heals. This is typical and suggests new tissue growing to heal the ulcer. Not all mouth ulcers acquire a white covering after healing, and their appearance depends on their size and location. If you have concerns about the healing process of a mouth ulcer, odd symptoms, or delayed healing time, visit a healthcare expert.
Do Mouth Ulcers Go Away Naturally?
Yes, most mouth ulcers heal without therapy. Minor aphthous ulcers, the most frequent kind of mouth ulcer, heal without scarring in 1-2 weeks. However, if the mouth ulcer lasts longer than 2 weeks, grows especially wide or painful, or is accompanied by other symptoms, it is advised to see a doctor. They can diagnose the ulcer, manage symptoms, and promote healing.