Gum Disease
Gum Disease Treatment In Bassendean
Are you dealing with the discomfort of tender, inflamed gums, or continually battling bad breath? If so, you might be facing the unwelcome reality of gum disease.
Gum disease is typically categorized into two stages – gingivitis, the milder form, and periodontitis, the more advanced and severe stage. Known as the primary culprit behind bad breath, tooth loss, and dental discomfort, treating gum disease promptly and effectively is crucial to restore your oral health and halt its progression.
At Spring Orchid Dental, we are recognized as leading experts in gum disease treatment, dedicated to providing top-quality general dental care to our patients. Don’t let gum disease dim your smile – reach out to us and let us help you regain your oral health.


What is Gum Disease Treatment?
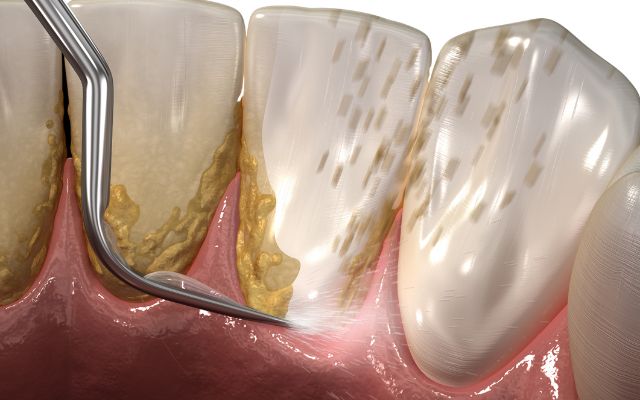
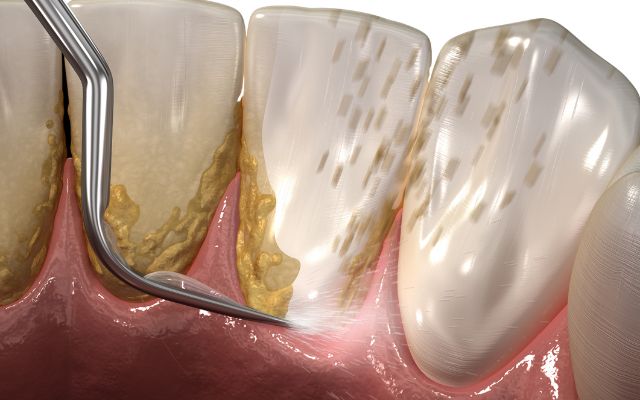
Gum disease treatment refers to the process of managing and remedying a group of conditions affecting the tissues surrounding the teeth, collectively known as periodontal diseases. Among these, Periodontitis stands out as a particularly detrimental condition instigated by the harmful accumulation of plaque on your teeth.
Plaque, a sticky deposit that clings to teeth, hosts a variety of bacteria. While some of these microorganisms are harmless, others can significantly deteriorate your gum health. Without regular, thorough brushing and proper flossing, plaque buildup intensifies, leading to gum irritation and eventually, periodontitis.
Get In Touch
Don’t let gum disease steal your smile! Contact Spring Orchid Dental in Bassendean today and schedule your gum disease treatment. It’s time to reclaim your oral health.
Common Symptoms
Here are some common symptoms associated with this condition:
- Tooth loss
- Pain in the mouth and teeth
- Receding, swollen, and painful gums
- Bleeding gums
- Pus between the teeth
- Sensitivity of the gums
- Improperly fitted dentures
- Mouth ulcers from brushing and flossing
- Bad breath
- Changes in your bite
- Discomfort during eating or chewing
- Tooth sensitivity
Who Need Gum Disease Treatment?
Gum disease treatment might be necessary for a variety of individuals depending on their oral health status and lifestyle factors. The following people are likely to require this treatment:
- People with poor oral hygiene
- Smokers and tobacco users
- Those with genetic predisposition
- Individuals with certain health conditions
- People with crooked teeth or ill-fitting dental restorations
- Those with symptoms of gum disease
- Medication users
- Older adults
Our Comprehensive Approach to Gum Disease Treatment
Consultation
The first step towards a healthy smile is a thorough consultation to assess your oral health and determine if you require periodontal cleaning or other treatments.
Hygiene Scaling
We employ advanced equipment for a thorough cleaning of the affected teeth. We offer various pain-relief options to ensure your visit is comfortable and stress-free.
Treatment Solutions
We provide non-surgical methods like antimicrobial treatments for plaque. When necessary, we perform periodontal surgery for comprehensive oral health restoration.
Review
We carefully monitor the healing process and recommend regular hygiene appointments to maintain optimal oral health and prevent the recurrence of gum disease.
Monday - Saturday: 9 AM – 5 PM
6/85 Walter Rd E Bassendean WA 6054
Choose Spring Orchid Dental For Your Treatment In Bassendean, Perth
Affordability
We strive to make superior dental care affordable. Despite our advanced treatment options and high-quality service, our prices are considerably more accessible than those of many other periodontal specialists.
Quality of Care
At Spring Orchid Dental, we take pride in our exceptional patient care. We ensure a comfortable and personalized experience for each patient, attentively addressing all your concerns and needs.
Surgical Expertise
With our state-of-the-art equipment, we can perform a comprehensive range of dental procedures in-house, negating the need for referrals to other specialists.
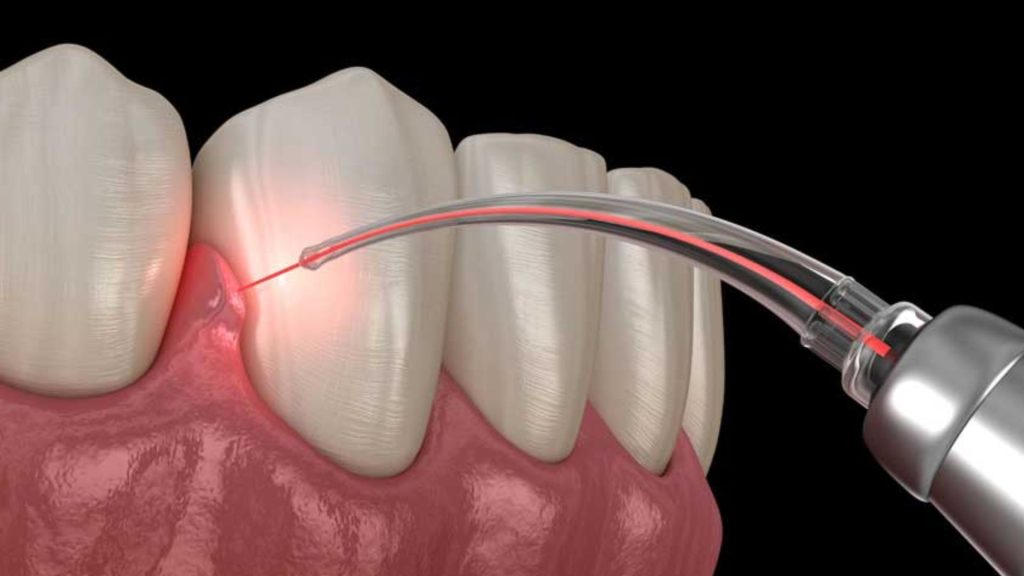
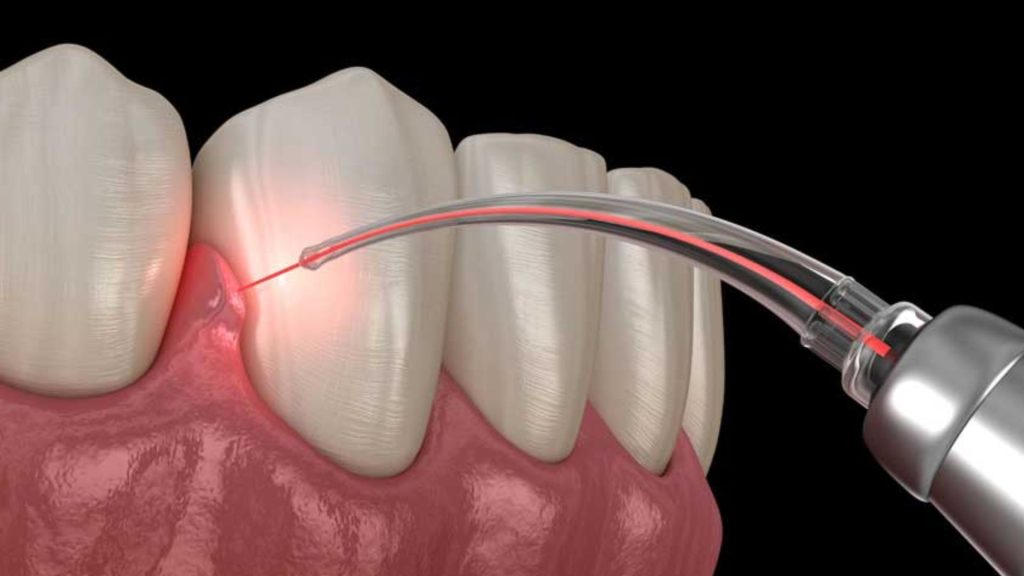
Cutting-Edge Technology
We leverage the latest technology in our treatments to provide you with the most accurate, efficient, and comfortable dental care experience.
FAQs
Is It Too Late To Save My Gums?
Gum disease can be treated at any time, and the extent of the treatment will rely on how advanced along it is.
How Fast Does Periodontitis Progress?
Periodontal disease progresses slowly but steadily. You will notice physical indications of gingivitis on day 5 because plaque only takes four days to reach its full extent. If you haven’t tried to treat the gingivitis, you can notice advanced stages of this disease in as little as a few weeks.
What Is The Best Treatment For Gum Disease?
Bacterial infection can be controlled with topical or oral antibiotics. Topical antibiotics can be applied topically, such as antibiotic mouthwashes, or they can be inserted into pockets after a deep cleaning to treat bacterial infections.
Can You Get Rid Of Gum Disease Completely?
Gum disease is treatable. Gum disease is treatable. It all boils down to eradicating bacteria from your mouth and allowing your gums to restore back to health. The first step in treating gum disease is to obtain the necessary knowledge so that you can effectively clean your teeth at home. Call us for more information.
How To Prevent Gum Disease?
To prevent gum disease occurs, you need take care of your oral health:
- Brush your teeth at least twice a day.
- Make sure the bristles of your toothbrush are soft, or even extra soft.
- Floss everyday.
- Utilize an organic mouthwash.
- To optimize your cleaning ability, use an electric toothbrush.
- Three-monthly toothbrush replacement.
- It’s recommended that everyone see a dentist every six months.